While diagnosis before 3 years of age is ideal, circumstances may not always allow the earliest identification and diagnosis. This week’s podcast explores two of the reasons why diagnosis is not always possible before age 3. One is a study from Denmark and one is from members of the Baby Siblings Research Consortium.
A new study from the ASF-supported Baby Siblings Research Consortium explains why a few kids with autism do not receive a formal diagnosis until 5 years or later. Read more here.
This week, ASF wants YOUR feedback on a new paper in the Journal of Autism and Developmental Disorders, which suggests that the reason there is so much discord in the autism community is that people with autism are just too different and have difficulties understanding each other’s perspective. Is this true? What do you think? Thanks to Becca Lory, CAS, BCCS for sharing! Listen to the podcast here.
Dr. Inna Fishman from San Diego State University explains how findings from brain tissue helps scientists interpret data which studies how brain regions connect to each other and why this is important for understanding autism subgroups. Also, researchers from the Karolinska Institutet examine ADHD diagnosed in adults, and find it is similar to autism. Listen to the podcast here.
This week, Dr. Mark Shen from The University of North Carolina at Chapel Hill explains new findings looking at the fluid around the brain. It’s now seen in families even without a family history of ASD, the finding has now been seen in different independent studies, including those at the UC Davis MIND Institute in California, it might be a diagnostic biomarker of ASD, and it also might help explain sleep problems. Hear more on this week’s podcast.
Today, ASF announced that it will be leading the newly-launched Alliance for Genetic Etiologies of Neurodevelopmental Disorders and Autism (AGENDA). This alliance is a partnership of research and advocacy organizations focused on improving outcomes of individuals with all forms of autism by fostering a genetics-first approach to autism science. AGENDA will also work to strengthen collaborations among organizations representing genetically-defined disorders associated with autism. As part of its collaborative activities, today AGENDA launched a new online portal that will make it easier for researchers to investigate different forms of autism. Clinicians, basic scientists, industry, and multiple end users of this information were consulted on the development of the portal, which along with contact information to access the data in each registry, can be found here.
This podcast is dedicated to siblings of people with autism who are typically developing. They play an important and beneficial role in development of socialization of those with ASD. But sadly, they also have issues of their own, such as a high rate of issues like anxiety and depression. Those siblings may be genetic carries of a specific mutation and not have an autism diagnosis, but have increased risk for schizophrenia and cognitive disability. Finally, just because they are considered “typically developing” doesn’t mean they don’t have challenges with adaptive behavior. However, they have a very special relationship with their brothers and sisters, and the world needs these strong advocates for the community.
Recently, Clare Harrop from University of North Carolina at Chapel Hill published two papers which help explain the differences between boys and girls with autism, at least in kids and toddlers. She graciously agreed to talk with ASF about these findings and what it means for better identification and diagnosis of girls with ASD, and where future research is needed, for this week’s podcast. Thank you to Dr. Harrop for this insight and for your work in this area!
This week’s ASF podcast focuses on how co-occuring conditions with autism, like anxiety, depression, and OCD, have changed over time. The increase in these conditions may help in defining different subgroups of autism. Listen on asfpodcast.org or on your favorite podcatcher!

Allyson Schwartzman at her graduation from Hofstra University School of Education.
By Allyson Schwartzman
When I was graduating from elementary school, someone on the yearbook committee asked me, “What do you want to be when you grow up?” I will never forget thinking for a moment and then stating “an autism teacher”. In my yearbook, there is a picture of me and under it says “an autism teacher”. You might be thinking this is a very interesting answer for a young child to give, but I had a good reason behind this answer. My twin brother, Robert, has autism and over our lives, I saw the progress he made with many thanks to his incredible teachers. I thought to myself, I would love to be just like them so I can help other children with autism. As I matured and got older, I realized this autism teacher job I wanted really meant that I wanted to be a special education teacher.
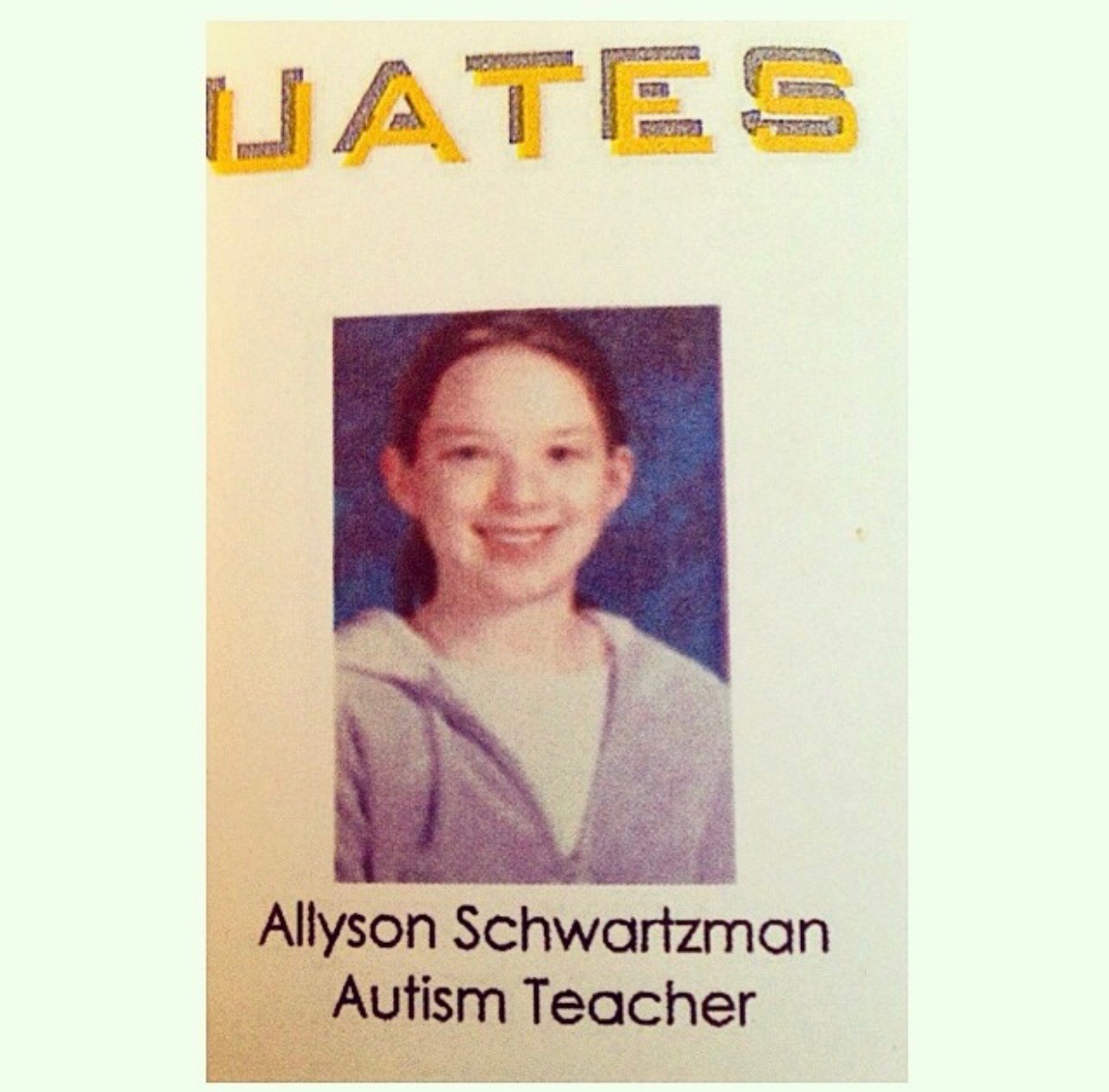
Allyson Schwartzman’s elementary school yearbook photo.
When I started college at Hofstra University, I was accepted into the School of Education. I graduated with my bachelor’s degree in Early Childhood and Childhood Education and eventually got a job as a Universal Pre-Kindergarten Teacher in a public school district on Long Island. I had this job for two years while in graduate school for my Master in Early Childhood Special Education and Intervention program, also at Hofstra University. I always knew I wanted to be a special education teacher, however, I had to decide on the age range of students I would work with. I decided to go down this route for my master’s because I fell in love with working with young children. There are so many developmental milestones that a teacher can help young children with disabilities reach. I love teaching and helping children grow their physical, intellectual, emotional, and social development through different fun and engaging activities. By being an early childhood special educator, I am able to accomplish these goals with a variety of different students.
After many endless nights of working and studying, I was able to accept my first position this year as an early childhood special education teacher in an integrated preschool. I finally accepted my dream job! I took a job in an integrated preschool setting specifically because I believe in the importance of integration and having students with disabilities learn with and from their peers. All children with disabilities need to be placed in the proper learning environment that works for them, and I am excited to work in this environment.

Collage of photos with Allyson Schwartzman and her twin brother, Robert.
I am so thankful that my brother Robert has influenced me to go down the path of special education. I am so proud of him and the progress he has made. He drives my dedication to this career choice everyday. It was definitely not an easy road getting here, but I cannot wait to make a difference in the lives of all the students I work with! I can now smile every time I look in my elementary school yearbook because I followed my dream. Now, I am living it.
This week’s podcast begins with a comment on the debate over ABA – helpful or harmful? But the big news this week is an analysis of very early, but very published, data on the use of MDMA, also known as “ecstasy” or “Molly”, in people with autism. Called an “empathogen”, MDMA can elicit feelings of warmth, love, and need to cuddle. However, it has a dark side. MDMA is a neurotoxin. It kills serotonergic brain cells. There is no known safe dose. Researchers studied and found weak evidence that it reduces social anxiety in people with autism. Social anxiety isn’t a core symptom of autism. Thank you to Dr. Larry Scahill of Emory University who provided an expert description of each condition. While ASF will not comment on every negative study out there, this one is worth noting.
When someone offers you MDMA, JUST SAY NO.
The following is the transcript of the ASF Weekly Science Podcast episode titled, “Can IGF-1 treat autism symptoms? A clinical trial aims to find out,” published on September 10, 2018. If you would like to learn more about the Mount Sinai clinical trial led by Dr. Alex Kolevzon, please go here.
Mahir Rahman (MR): Hello, everyone, this is Mahir Rahman. Welcome to the Autism Science Foundation Weekly Science Podcast. I’m subbing in for Alycia for an interview I conducted with Dr. Alex Kolevzon of Mount Sinai. Hope you enjoy the story.

Faculty members of Dr. Kolevzon’s lab at the Seaver Autism Center (left to right): Danielle Halpern, PsyD; Jennifer Foss-Feig, PhD; Paige Siper, PhD; Alex Kolevzon, MD; Pilar Trelles, MD; Michelle Gorenstein, PsyD
MR: A Mount Sinai research team led by Dr. Alex Kolevzon is investigating if a compound known as insulin-like growth factor 1, also known as IGF-1, can be used as a treatment for autism. Dr. Kolevzon is a child psychiatrist and the clinical director of the Seaver Autism Center in the Icahn School of Medicine at Mount Sinai in New York. He received the Autism Science Foundation Treatment Grant in 2013. He sat down with ASF to discuss his current study. We began the interview by discussing the autism-related disorder Phelan-McDermid syndrome, also known as PMS.
Alex Kolevzon (AK): Phelan-McDermid syndrome is a neurodevelopmental disorder that causes autism. It is due to a deletion or mutation of the SHANK3 gene, which is located at the terminal end of chromosome 22. There’s two copies of the SHANK3 gene, we all have two copies of it. And so, in Phelan-McDermid syndrome, you’re basically missing one copy and that’s called haploinsufficiency.
MR: Are you wondering what happens if you miss one copy of the SHANK3 gene? Well, SHANK3 is a gene that codes for a protein that helps brain cells communicate with each other in order to make useful connections during development. When one copy of the SHANK3 gene is missing, certain brain cells cannot communicate with each other, leading to a number of problems.
AK: So based on very large genetic studies, it seems as if Phelan-McDermid syndrome or SHANK3 deletions and mutations account for about 1% of autism, and not everyone with Phelan-McDermid Syndrome has autism, so there’s going to be additional cases beyond that. So really it’s very common. We’re just now starting to routinely diagnose people.
MR: How can some kids with PMS have autism and others not?
AK: Well, autism is a behavioral diagnosis. It’s really just a collection of symptoms, social impairments, language impairments, restricted and repetitive behaviors, and, you know, many different people with autism look very, very different. So some kids have… with Phelan-McDermid syndrome have a lot of social motivations, social interests, social engagements. And despite being significantly cognitively delayed, the social domain is a relative strength for them, and as a result, they don’t really meet the criteria for an autism spectrum disorder. We’re talking about maybe 15% to 20% of them. So the vast majority of people with Phelan-McDermid syndrome do meet the criteria for autism. But it’s important to understand that if you take a given biological cause of a syndrome, the clinical features of that syndrome could be very, very wide.
MR: To reiterate, it’s important to understand that, like autism, the symptoms of PMS can vary. They can vary enough that some children with PMS don’t meet the criteria for an autism diagnosis, but most of the time, they will. That said, the symptoms seen in autism might be based on biology similar to that of PMS.
AK: Within the broader universe of people with autism, and especially people with autism where there isn’t a known cause — what we call idiopathic autism, it seems as those a subset of them appear clinically, and even on some biological measures, look like people with Phelan-McDermid syndrome.
MR: If two conditions have similar biology, the same treatment may be able to help both. The search for a treatment for PMS and idiopathic autism led Dr. Kolevzon’s team to a group of compounds known as growth factors. Growth factors can help cells grow, change, and make new connections, what scientists call plasticity.
AK: A growth factor can promote growth, promote synaptic plasticity, which is what is essentially absent in Phelan-McDermid syndrome. So we started doing this study with a drug called insulin-like growth factor, which we know crosses into the brain, we know it promotes synaptic maturity, synaptic plasticity, nerve cell growth, and we did a couple of small studies, both of which were very, very promising.
MR: In a pilot clinical trial using IGF-1, Dr. Kolevzon’s team found children with PMS tolerated the drug. They also found that the children treated with IGF-1 had reduced expression of two core symptoms of autism – social withdrawal and repetitive behaviors.
AK: We looked at social symptoms and repetitive behavior symptoms because those are core domains of autism. And those are both studied in this trial using a parent-report measure, and we saw improvement in both those domains in the trial with IGF-1.

Dr. Kolevzon’s lab during a team meeting.
MR: Dr. Kolevzon’s team made sure every participant had the opportunity to receive the IGF-1 treatment in the trial by employing a crossover design.
AK: Patients got drugs for 12 weeks, or placebo, and they switched to the other condition, so each patient essentially acted as their own control and treatment was for 12 weeks and placebo was for 12 weeks in random order. We applied the exact same design to the trial in idiopathic autism.
MR: Employing a crossover design was an intentional decision by his team.
AK: One of the biggest obstacles to success in clinical trials is recruitment. One of the biggest obstacles to families wanting to participate is the idea of being on placebo and not getting access to the active treatment. So we purposely designed the trial with everyone getting active treatment.
MR: Based on the findings made by Dr. Kolevzon’s team, IGF-1 appears to be a safe treatment that offers notable improvements in core symptoms of autism, so why is it not considered an effective treatment yet? Dr. Kolevzon hopes to address that question with his current study.
AK: The fear in the field in general is we might be studying an effective medicine but we are not able to show improvement because our measures are not ideal. Either we’re not measuring the right thing, measures aren’t sensitive enough, we’re not able to really account for the placebo effect because they’re so biased. So we’ve been focusing a lot more on more objective, more quantifiable measures, trying to develop new ways of looking at symptoms.
MR: His current study is focusing on sensory reactivity symptoms. Many people with PMS and autism have sensory issues, including varying sensitivity to light and sound and atypical interests in specific textures and temperatures. In order to examine brain activity in general and during periods of sensory reactivity, his lab uses a technique called electroencephalography, or EEG. Dr. Kolevzon’s team will be examining how IGF-1 affects sensory reactivity and brain activity following IGF treatment
AK: That’s really an important symptom, it’s a symptom that’s virtually universal. All kids with Phelan-McDermid syndrome, at least all the kids that we have evaluated, have some sensory reactivity symptoms. Often, they are hyporeactive.
MR: Meaning that these kids often have a decreased response to sensory stimuli. Say a child with sensory hyporeactivity entered a room with very loud speakers. The child might not be bothered by, or let alone react to, the volume. With IGF-1 treatment, Dr. Kolevzon believes his team will be able to observe any change of those sensory reactivity symptoms over the course of the clinical trial.
AK: This is a trial that is pretty burdensome for families because the way that IGF-1 is delivered is through subcutaneous injection. So families are taught to monitor their children’s glucose levels because one of the main side effects can be low blood sugar, and they’re also taught how to inject the children twice a day with small amounts of IGF-1. It’s a very, very small needle and actually, it’s probably the element of the study that people are most concerned about when they first consider it, and it ends up in actually 19 out of 19 cases not to be a really big issue. The children, because they have the sensory hyporeactivity, aren’t especially averse to the shots and the parents become remarkably expert very, very quickly. We give them a big manual with lots of instructions. We show them exactly how big, and in this case, how tiny the needle is, but then, the very first day that they actually get the injection, I give it to them myself.
MR: Dr. Kolevzon and his team understand that they’re asking a lot from the families choosing to participate in the study. They take great strides in order to prepare and help the families throughout the recruitment and trial process.
AK: For me to say things like, “Oh, this is not a big deal,” isn’t helpful. Obviously, this is a big deal, we acknowledge that on the onset, but for me to also encourage them and say, “Look, it’s going to feel scary and then you’re going to be quite good at it.” That’s one thing. I think the other thing is that they don’t feel alone in this, right? They don’t have to make decisions on their own. They don’t have to worry about dosing on their own. You know, if they see anything concerning, they don’t need to decide what to do about that. They have unfettered access to me. We exchange cell phone numbers early on and then, the other thing I say to them is, “You know, if you have any concerns at all, skip the dose. That’s it. You get to control that. If you don’t want to give your child the does for whatever reason, just skip the dose. There will not be any harm in that.” Then, we just take it from there.
MR: For those autism families that are listening, Dr. Kolevzon has a message for you.
AK: “Come participate!” I’d say that if you’re not convinced that a clinical trial is a good idea, that’s okay also. Come just to get to know us. Let us get to know you. And then, you know, we’ll figure it out. Nobody has ever required anybody to participate in a clinical trial. We definitely respect how scary it can be and how hard it can be. So it’s really all about just the fit.
MR: You can learn more about this study on asfpodcast.org. Thanks for listening.

