Written by staff and the SAB of the Autism Science Foundation

COVID Recovery Was Slow, But Scientific Progress Continues
After two grueling pandemic years, 2022 saw a return to quasi-normalcy in both the world at large and in the world of autism research. Although the pandemic was incredibly challenging for autism families and researchers, the pivot to telehealth led to advances in online autism diagnoses, mental health supports, and interventions that will likely benefit autistic people across the globe for years to come.
Autism scientists working in diverse areas of research made important strides this year and continued to gain valuable insights into every facet of autism. They also identified more effective ways to support people on the spectrum. Researchers developed a better understanding of the unique needs and priorities of specific groups of autistic people, better-defined links between biological mechanisms and behavior, and disparities in autism diagnosis and treatment.
This work was only possible because of families like yours: You actively participated in important research studies. You agreed to have your data shared with others. You donated. You advocated. Your U.S. tax dollars supported $100 million of NIH grants funded in 2022.

Autism science simply cannot progress without your continued partnership. Earlier this year, ASF launched a “Participate in Research” directory to match families with research studies that meet your needs and interests. Many of these studies offer compensation, and can also provide valuable information and resources to aid your family member. The goal is to use the information gleaned from research to improve the real lives of real people, both now and in the future.
Here’s a little bit of what 2022 taught us.
Early identification leads to earlier diagnosis, but diagnosis happens at all ages
- Developmental milestones are skills that most children reach at a certain age and are used by healthcare providers to track progress. This year, the CDC updated these milestones to track what 75% of children can do by certain ages, rather than 50%, causing some pushback. In addition, the CDC added new time points as well as markers that might predict an autism diagnosis.1
- In autism, reaching developmental milestones can be delayed from months to years. Delays are often more severe and variable in those with co-occurring intellectual disability and a rare genetic variant. New research reinforced the need to focus on milestones and the importance of early intervention.: If you notice your infant is struggling with new skills, tell your healthcare provider.2
- Language skills in infants are an important predictor of an ASD diagnosis. Recent work from the ASF-supported Baby Siblings Research Consortium (BSRC) showed that maternal education levels and early gestures are important predictors of these language skills, suggesting markers for intervention.3
- Researchers have suggested that early behaviors that are predictive of a later diagnosis may be part of a larger “developmental cascade,” where, for example, the trajectory from laying to sitting to language may be disrupted. These are intertwined behavioral and neurobiological networks that affect how a person with autism functions.4
- There are now multiple biomarkers under investigation. Some are better than others at not just autism diagnosis, but the response to intervention.5 In the future, they can be used to promote earlier diagnosis and more objective measures of the effectiveness of interventions.
Key takeaways: Parents and clinicians should monitor developmental milestones early in life. Early signs are not a substitute for a diagnosis, but some supports and interventions can be provided that allow for an improvement of trajectories across the lifespan.
Parent-mediated interventions and training – they work!
- A review of 30 studies showed promising results from parent-mediated interventions, but improvements in studies are still needed.6
- Parent-mediated interventions can be used for teaching everything from core autism symptoms to self-care like tooth brushing.7
- Autism interventions can and should be customized to culture and race.8,9
- Some parent-mediated interventions have been tested successfully in a hybrid format, leading the way for others to investigate their effect on parent and child outcomes.10
- While some have suggested parents only recognize the weaknesses in their children, recent research strongly notes that parents know their child’s strengths and use those strengths to help support their family. Educators also note these strengths in the classroom.11,12
- Siblings play an important role in the outcome of autistic individuals, while they also experience unique challenges themselves.13,14
Key takeaways: Parents and caregivers often feel helpless when they are concerned about their child’s development and are facing long waiting lists for services. New research shows that providing support is beneficial for both the parents and the child outcome, and elevates strengths while mitigating support challenges. Further research should continue to explore the role of sibling relationships and support.
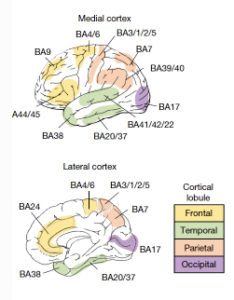
The brain has a distinct “signature” and sensory issues are on the front line
- One type of immune cell of the brain called the microglia has been known to affect cell communication, shape, and number. Researchers have now determined when and where these cells are expressed during development, laying the foundation for research into a critical brain cell type.17
- The greatest differences in gene expression in the brain are in sensory areas like the visual cortex.15 This may explain the almost universal problems in sensory processing that autistic individuals experience, and why sensory problems are so common in ASD.18
- The visual area, specifically the occipital cortex, was also enlarged at young ages, more so in kids who have siblings with a diagnosis, demonstrating that genetic heritability plays a role in brain activity involved in sensory processing in families.19
- A new marker of sensory processing was detected: differences in the activity of a neurotransmitter called GABA. GABA commonly slows down the activity of brain cells, which is important when they are too active, indicating this neurotransmitter is critical for sensory processing. Changing the activity of GABA neurons can alleviate sensory problems in autistic individuals.20
- In addition, changes in the thickness of different cortical regions may influence sensory responses, depending on whether there is overstimulation or understimulation.21
- Another brain region called the amygdala may relate to anxiety in autistic people. Certain areas of the amygdala are different in size,22 and can explain variability in anxiety.23 There is also disruption in connectivity from the amygdala to outside regions,24 which may also explain how anxiety interacts with autism features.
- Rather than examining one autism feature at a time, it seems that ability to make gains or show potential for change over time is correlated to differences in brain structure. Markers of change over time are also linked to genes associated with ASD.25 Targets of intervention based on biological markers may need to focus on sensitivity to change rather than a specific number on an instrument per se.
- The use of biological tools has increased this year. These tools include induced pluripotent stem cells (IPSCs) and organoids that are based on cells from individuals with different forms of ASD. Studies have looked at different types of autism (idiopathic and genetically-based) and identified creation of new brain cells as a common biological mechanism.26 New studies also used novel tools to improve the validity of these cell-based systems.27
- Animal models can be used to identify mechanisms by which genes and environmental factors exert their influence over behavior. Right now, there are hundreds of animal models of ASD, but not all of them are used appropriately to understand ASD. The ability of the model to recapitulate both the biology and behavior involved in ASD is essential.28
Key takeaways: While different brain regions are specialized in their function, they interconnect and turn on and off in synchrony. Researchers need better models of human neurobiology, including better animal models, to understand the core and associated autism features, from sensory dysfunction to GI issues. If you want to learn more about research involving the brains of people with autism, sign up for more information at Autism BrainNet.
Genetic markers start to explain phenotype

- The presence of rare genetic variants and common variants tend to funnel people into groups defined by intellectual disability (ID) or high educational attainment.29,30 Scientists have identified and characterized two major types of genetic variation associated with ASD. Rare genetic variants are commonly associated with lower cognitive function and profound autism, but that is not always the case.31 Even with hundreds of thousands of samples, scientists have still not found a direct gene – outcome linkage. However, genetics are still important. Genetic findings can help identify specific needs leading to appropriate supports.
- Certain types of gene mutations can explain associations with features like psychosis,32 as well as obesity and depression.33
- Five new variants were identified that are not linked to intellectual or developmental disability (IDD), but are linked to other neuropsychiatric issues besides ASD.31,34 Therefore, rare ASD or DD gene mutations usually lead to some sort of deleterious outcome.
- There is a significant overlap between ASD genes and genes associated with developmental disorders in general. Researchers suggest that autism specificity may be the result of when the gene is expressed. For example, in developmental disorders, genes are expressed in progenitor cells while in ASD they may be expressed in developing neurons.35
- Other studies have not found any ASD-specific gene, they show linkage to neurodevelopmental problems in general, and can be grouped based on what cells are affected.35
- There are shared pathways between ASD and other neuropsychiatric disorders.36
- Studies have shown linkages between epilepsy, ASD and ADHD.37
Key takeaways: Genetic markers associated with ASD are also associated with other developmental conditions like ADHD and intellectual disability, as well as comorbid conditions like obesity. Two major types of genetic markers, rare and common variations, may represent biomarkers of two different phenotypes, but there is overlap, and rare and common variants are likely mixed in most people. Genetic research is important for a better understanding of ASD and the development of individualized approaches for supports.
But genetics doesn’t tell it all
- Parental genetics and environmental factors are intertwined on a biological level. Genes associated with depression in parents are also linked to ASD.38
- Maternal immune infections are an established risk factor for ASD. However, the genetics of children with and without maternal immune challenges during pregnancy are different.39
- Studies in Norway offer a unique perspective of gestational exposures by banking blood taken mid-pregnancy during usual obstetrical visits. One study has shown that certain cytokines, or markers of immune activity, are elevated during pregnancy in both boys and girls with autism, particularly in girls. It’s unclear what role these cytokines play collectively or individually, or where they came from in the first place.40
- Where you live can affect the role of genes vs. environment, evidenced by environmental factors playing a bigger role in heritability in certain areas of Sweden and the U.K.41
- Genetics and the environment clearly interact when it comes to the influence of an ASD diagnosis. For example, pesticide exposure exacerbated the effects of the autism CHD8 gene on rodent behavior.42
- The role of environmental factors may depend not just on a diagnosis but on specific autism traits.43
- Given that autism is likely part of a larger developmental disorder spectrum, regulation of toxic chemicals which are harmful to development must be expanded.44
Key takeaways: The role of environmental factors in ASD has often been disassociated with genetics when it should be integrated into the understanding of autism’s causes, behavioral features, and interventions.
Biological sex plays a role

- Studies replicated this year showed that females with autism have a higher burden of rare genetic mutations. In addition, research is demonstrating that females with an autism diagnosis also show a higher level of “common” variations.29,45
- The effect of higher levels of common variation in females extends to even undiagnosed members of ASD-impacted families, demonstrating that females carrying ASD genetic variation are resilient.45
- The two above studies implicate an important role of the female protective effect but do not explain all of the differences in diagnosis.46
- Some scientists have wondered if biases in instruments used to inform a diagnosis play a role in the sex difference. One study used a mathematical algorithm to eliminate the difference in M:F diagnostic differences, but still, females show different behavioral profiles. This further reiterates that instruments should be used to inform, not make a diagnosis, and that autism is more than a yes or no diagnosis. 47
- Clinicians may miss an autism diagnosis in females because of camouflage. Females are also more likely to camouflage, which means they (consciously or unconsciously) pretend to fit in as a typically-developing girl. This leads to lower quality of life.48
- Intellectual disability plays a bigger role in autism features in girls vs. boys.49
- New genetic mutations involving the X chromosome were identified – and these mutations are more likely to occur in females.35
- Sex differences in brain region size can be attributed to gene expression patterns. In other words, brain differences in males and females with ASD are due, in part, to underlying genetics.50
Key takeaways: Females with ASD show different biological and behavioral profiles and are understudied in research and underserved in the community. Future research should aim to include more females to better understand their unique needs and provide targeted support.
It’s still not over, but families are in a better place than a year ago
- Despite a rocky start at the height of the pandemic in 2020 and 2021, opportunities to receive autism diagnoses, mental health supports, and interventions via telehealth have been improved, and polished, and are not only acceptable to families and clinicians but are effective.51-57
- Families and clinicians were happier with remote diagnosis and evaluation when the diagnosis was clear; in cases where there was some ambiguity, it caused frustration.58,59
- While many families and individuals experienced a mental health decline during the pandemic, some exhibited resiliency under social distancing guidelines.60 The differences could be due to the degree to which services were lost, coping styles, and pre-existing mental health attributes.61
Key takeaways: Autism families suffered during the pandemic, but it also allowed for new approaches to be developed that may ultimately improve practice – including hybrid clinical services, holistic family support, and more comprehensive diagnostic practices.
It’s not all about the ASD
- Individuals with ASD experience higher levels of anxiety, GI issues, epilepsy, and other developmental disorders like ADHD compared to those without a diagnosis.
- While not a core autism symptom, anxiety is linked to insistence on sameness in toddlers with ASD, which indicates a similar underlying mechanism.62
- Gastrointestinal issues plague people with autism, and there are few options for treatment. The gastrointestinal microbiome has been a target for intervention for autism symptoms, although studies are still ongoing.63 GI issues were the focus of a major NIH-funded meeting this year.
- Suicide risk is higher in ASD. 64
- Sleep problems, while mostly studied in children, are now shown to follow kids into adolescence and adulthood.65
- There is a high degree of overlap in the brain activity profiles between ADHD and ASD kids. Differences are mostly seen when symptom severity is accounted for. ADHD and ASD show more similarities in the brain than differences.66
- Behavioral profiles between ADHD and ASD are also similar.67
- Mental health concerns are present in adolescents and adults with ASD with cognitive inflexibility strongly linked to compromised mental health.68,69 Cognitive inflexibility, which is different than cognitive ability, is how someone shifts their attention from one thing to another based on what is going on around them. This may be a focus for future mental health interventions.
- Unfortunately there are no strong individual-level predictors in childhood of mental health issues in adults, but some factors that may lead to better mental health are better living skills and higher IQ.70
Key takeaways: Outside the core features of autism listed in the DSM5, individuals experience a wide range of associated features, ranging from psychiatric issues to medical comorbidities. For many individuals, these associated features are highly debilitating.
Biases in underserved communities are getting more attention

- A recent analysis showed a reduction of the disparities in the age of ASD diagnosis for Black and Hispanic children over the last four years, but a difference still exists.71
- This is likely due to provider bias, but not necessarily diagnostic instrument biases. The standard diagnostic tools are not biased toward race or sex.72
- Lessons learned from the pandemic reiterate the need for intense community engagement, flexibility, and an understanding that a holistic approach – rather than one focused on ASD – is necessary for working with underserved communities73,74.
- A culturally-adapted parent training program delivered by Black providers was effective in the Black community and could be a model for future engagement efforts.8
- Only 25% of intervention studies report the ethnic and racial makeup of their participants,75 indicating that researchers need to do a better job of deliberately including racial and ethnic minorities, recruiting them as research leads and coordinators, and including them on boards for scientific review.76
- Low socioeconomic status contributes to social and communication deficits in young children with ASD.77
Key takeaways: Racial and ethnic biases are still pervasive in autism research and diagnosis, and we need a holistic approach to support families in all aspects of their lives beyond just autism symptoms. Scientists must continue to focus on the deliberate inclusion of these groups in both research and career training to better serve all individuals with autism.
On a final note, there has been a lot of debate this year about the language used to describe autism. 78-81 There is a diversity of experiences with autism and likely to be a diversity of perspectives. Families and scientists should use scientifically accurate terms to best describe the wide range of autistic people and their symptoms.82 What that is may differ from person to person, and situation to situation, which means context and preference need to be considered as well.
References
1. Zubler JM, Wiggins LD, Macias MM, et al. Evidence-Informed Milestones for Developmental Surveillance Tools. Pediatrics 2022; 149(3).
2. Kuo SS, van der Merwe C, Fu JM, et al. Developmental Variability in Autism Across 17 000 Autistic Individuals and 4000 Siblings Without an Autism Diagnosis: Comparisons by Cohort, Intellectual Disability, Genetic Etiology, and Age at Diagnosis. JAMA Pediatr 2022; 176(9): 915-23.
3. Pecukonis M, Young GS, Brian J, et al. Early predictors of language skills at 3 years of age vary based on diagnostic outcome: A baby siblings research consortium study. Autism Res 2022; 15(7): 1324-35.
4. Bradshaw J, Schwichtenberg AJ, Iverson JM. Capturing the complexity of autism: Applying a developmental cascades framework. Child Dev Perspect 2022; 16(1): 18-26.
5. Webb SJ, Naples AJ, Levin AR, et al. The Autism Biomarkers Consortium for Clinical Trials: Initial Evaluation of a Battery of Candidate EEG Biomarkers. Am J Psychiatry 2022: appiajp21050485.
6. Conrad CE, Rimestad ML, Rohde JF, et al. Parent-Mediated Interventions for Children and Adolescents With Autism Spectrum Disorders: A Systematic Review and Meta-Analysis. Front Psychiatry 2021; 12: 773604.
7. Fenning RM, Butter EM, Macklin EA, et al. Parent Training for Dental Care in Underserved Children With Autism: A Randomized Controlled Trial. Pediatrics 2022; 149(5).
8. Kaiser K, Villalobos ME, Locke J, Iruka IU, Proctor C, Boyd B. A culturally grounded autism parent training program with Black parents. Autism 2022; 26(3): 716-26.
9. Rivera-Figueroa K, Marfo NYA, Eigsti IM. Parental Perceptions of Autism Spectrum Disorder in Latinx and Black Sociocultural Contexts: A Systematic Review. Am J Intellect Dev Disabil 2022; 127(1): 42-63.
10. Brian J, Solish A, Dowds E, et al. “Going Mobile”-increasing the reach of parent-mediated intervention for toddlers with ASD via group-based and virtual delivery. J Autism Dev Disord 2022; 52(12): 5207-20.
11. Mirenda P, Zaidman-Zait A, Cost KT, et al. Educators Describe the “Best Things” About Students with Autism at School. J Autism Dev Disord 2022.
12. Wilkinson E, Vo LTV, London Z, Wilson S, Bal VH. Parent-Reported Strengths and Positive Qualities of Adolescents and Adults with Autism Spectrum Disorder and/or Intellectual Disability. J Autism Dev Disord 2022; 52(12): 5471-82.
13. Rosen NE, Schiltz HK, Lord C. Sibling Influences on Trajectories of Maladaptive Behaviors in Autism. J Clin Med 2022; 11(18).
14. Mokoena N, Kern A. Experiences of siblings to children with autism spectrum disorder. Front Psychiatry 2022; 13: 959117.
15. Gandal MJ, Haney JR, Wamsley B, et al. Broad transcriptomic dysregulation occurs across the cerebral cortex in ASD. Nature 2022; 611(7936): 532-9.
16. Chen Y, Dai J, Tang L, et al. Neuroimmune transcriptome changes in patient brains of psychiatric and neurological disorders. Mol Psychiatry 2022.
17. Menassa DA, Muntslag TAO, Martin-Estebane M, et al. The spatiotemporal dynamics of microglia across the human lifespan. Dev Cell 2022; 57(17): 2127-39 e6.
18. Wiggins LD, Tian LH, Rubenstein E, et al. Features that best define the heterogeneity and homogeneity of autism in preschool-age children: A multisite case-control analysis replicated across two independent samples. Autism Res 2022; 15(3): 539-50.
19. Girault JB, Donovan K, Hawks Z, et al. Infant Visual Brain Development and Inherited Genetic Liability in Autism. Am J Psychiatry 2022; 179(8): 573-85.
20. Huang Q, Pereira AC, Velthuis H, et al. GABA(B) receptor modulation of visual sensory processing in adults with and without autism spectrum disorder. Sci Transl Med 2022; 14(626): eabg7859.
21. Habata K, Cheong Y, Kamiya T, et al. Relationship between sensory characteristics and cortical thickness/volume in autism spectrum disorders. Transl Psychiatry 2021; 11(1): 616.
22. Seguin D, Pac S, Wang J, et al. Amygdala subnuclei volumes and anxiety behaviors in children and adolescents with autism spectrum disorder, attention deficit hyperactivity disorder, and obsessive-compulsive disorder. Hum Brain Mapp 2022; 43(16): 4805-16.
23. Andrews DS, Aksman L, Kerns CM, et al. Association of Amygdala Development With Different Forms of Anxiety in Autism Spectrum Disorder. Biol Psychiatry 2022; 91(11): 977-87.
24. Lee JK, Andrews DS, Ozturk A, et al. Altered Development of Amygdala-Connected Brain Regions in Males and Females with Autism. J Neurosci 2022; 42(31): 6145-55.
25. Pretzsch CM, Schafer T, Lombardo MV, et al. Neurobiological Correlates of Change in Adaptive Behavior in Autism. Am J Psychiatry 2022; 179(5): 336-49.
26. Connacher R, Williams M, Prem S, et al. Autism NPCs from both idiopathic and CNV 16p11.2 deletion patients exhibit dysregulation of proliferation and mitogenic responses. Stem Cell Reports 2022; 17(6): 1380-94.
27. Revah O, Gore F, Kelley KW, et al. Maturation and circuit integration of transplanted human cortical organoids. Nature 2022; 610(7931): 319-26.
28. Silverman JL, Thurm A, Ethridge SB, et al. Reconsidering animal models used to study autism spectrum disorder: Current state and optimizing future. Genes Brain Behav 2022; 21(5): e12803.
29. Antaki D, Guevara J, Maihofer AX, et al. A phenotypic spectrum of autism is attributable to the combined effects of rare variants, polygenic risk and sex. Nature Genetics 2022; 54(9): 1284-92.
30. Warrier V, Zhang X, Reed P, et al. Genetic correlates of phenotypic heterogeneity in autism. Nature Genetics 2022; 54(9): 1293-304.
31. Zhou A, Cao X, Mahaganapathy V, et al. Common genetic risk factors in ASD and ADHD co-occurring families. Hum Genet 2022.
32. Brownstein CA, Douard E, Mollon J, et al. Similar Rates of Deleterious Copy Number Variants in Early-Onset Psychosis and Autism Spectrum Disorder. Am J Psychiatry 2022; 179(11): 853-61.
33. Birnbaum R, Mahjani B, Loos RJF, Sharp AJ. Clinical Characterization of Copy Number Variants Associated With Neurodevelopmental Disorders in a Large-scale Multiancestry Biobank. JAMA Psychiatry 2022; 79(3): 250-9.
34. Shimelis H, Oetjens MT, Walsh LK, et al. Prevalence and Penetrance of Rare Pathogenic Variants in Neurodevelopmental Psychiatric Genes in a Health Care System Population. American Journal of Psychiatry 2022: appi.ajp.22010062.
35. Wang T, Kim CN, Bakken TE, et al. Integrated gene analyses of de novo variants from 46,612 trios with autism and developmental disorders. Proc Natl Acad Sci U S A 2022; 119(46): e2203491119.
36. Murtaza N, Cheng AA, Brown CO, et al. Neuron-specific protein network mapping of autism risk genes identifies shared biological mechanisms and disease-relevant pathologies. Cell Rep 2022; 41(8): 111678.
37. Carson L, Parlatini V, Safa T, et al. The association between early childhood onset epilepsy and attention-deficit hyperactivity disorder (ADHD) in 3237 children and adolescents with Autism Spectrum Disorder (ASD): a historical longitudinal cohort data linkage study. Eur Child Adolesc Psychiatry 2022.
38. Havdahl A, Wootton RE, Leppert B, et al. Associations Between Pregnancy-Related Predisposing Factors for Offspring Neurodevelopmental Conditions and Parental Genetic Liability to Attention-Deficit/Hyperactivity Disorder, Autism, and Schizophrenia: The Norwegian Mother, Father and Child Cohort Study (MoBa). JAMA Psychiatry 2022; 79(8): 799-810.
39. Nudel R, Thompson WK, Borglum AD, et al. Maternal pregnancy-related infections and autism spectrum disorder-the genetic perspective. Transl Psychiatry 2022; 12(1): 334.
40. Che X, Hornig M, Bresnahan M, et al. Maternal mid-gestational and child cord blood immune signatures are strongly associated with offspring risk of ASD. Mol Psychiatry 2022; 27(3): 1527-41.
41. Reed ZE, Larsson H, Haworth CMA, et al. Mapping the genetic and environmental aetiology of autistic traits in Sweden and the United Kingdom. JCPP Adv 2021; 1(3): e12039.
42. Jimenez JA, Simon JM, Hu W, et al. Developmental pyrethroid exposure and age influence phenotypes in a Chd8 haploinsufficient autism mouse model. Sci Rep 2022; 12(1): 5555.
43. Isaksson J, Ruchkin V, Aho N, Lundin Remnelius K, Marschik PB, Bolte S. Nonshared environmental factors in the aetiology of autism and other neurodevelopmental conditions: a monozygotic co-twin control study. Mol Autism 2022; 13(1): 8.
44. Volk HE, Ames JL, Chen A, et al. Considering Toxic Chemicals in the Etiology of Autism. Pediatrics 2022; 149(1).
45. Wigdor EM, Weiner DJ, Grove J, et al. The female protective effect against autism spectrum disorder. Cell Genomics 2022; 2(6): 100134.
46. Dougherty JD, Marrus N, Maloney SE, et al. Can the “female protective effect” liability threshold model explain sex differences in autism spectrum disorder? Neuron 2022; 110(20): 3243-62.
47. Burrows CA, Grzadzinski RL, Donovan K, et al. A Data-Driven Approach in an Unbiased Sample Reveals Equivalent Sex Ratio of Autism Spectrum Disorder-Associated Impairment in Early Childhood. Biol Psychiatry 2022; 92(8): 654-62.
48. Ross A, Grove R, McAloon J. The relationship between camouflaging and mental health in autistic children and adolescents. Autism Res 2022.
49. Saure E, Castren M, Mikkola K, Salmi J. Intellectual disabilities moderate sex/gender differences in autism spectrum disorder: a systematic review and meta-analysis. J Intellect Disabil Res 2022.
50. Floris DL, Peng H, Warrier V, et al. The Link Between Autism and Sex-Related Neuroanatomy, and Associated Cognition and Gene Expression. American Journal of Psychiatry 2022: appi.ajp.20220194.
51. Rosen V, Blank E, Lampert E, et al. Brief Report: Telehealth Satisfaction Among Caregivers of Pediatric and Adult Psychology and Psychiatry Patients with Intellectual and Developmental Disability in the Wake of Covid-19. J Autism Dev Disord 2022; 52(12): 5253-65.
52. Talbott MR, Lang E, Avila F, Dufek S, Young G. Short report: Experiences of Caregivers Participating in a Telehealth Evaluation of Development for Infants (TEDI). J Autism Dev Disord 2022; 52(12): 5266-73.
53. Adler EJ, Schiltz HK, Glad DM, et al. Brief Report: A Pilot Study Examining the Effects of PEERS(R) for Adolescents Telehealth for Autistic Adolescents. J Autism Dev Disord 2022; 52(12): 5491-9.
54. Estabillo JA, Moody CT, Poulhazan SJ, Adery LH, Denluck EM, Laugeson EA. Efficacy of PEERS(R) for Adolescents via Telehealth Delivery. J Autism Dev Disord 2022; 52(12): 5232-42.
55. Jones E, Kurman J, Delia E, et al. Parent Satisfaction With Outpatient Telemedicine Services During the COVID-19 Pandemic: A Repeated Cross-Sectional Study. Front Pediatr 2022; 10: 908337.
56. Ferrante C, Sorgato P, Fioravanti M, et al. Supporting Caregivers Remotely During a Pandemic: Comparison of WHO Caregiver Skills Training Delivered Online Versus in Person in Public Health Settings in Italy. J Autism Dev Disord 2022: 1-20.
57. McNally Keehn R, Enneking B, Ryan T, et al. Tele-assessment of young children referred for autism spectrum disorder evaluation during COVID-19: Associations among clinical characteristics and diagnostic outcome. Autism 2022: 13623613221138642.
58. Klaiman C, White S, Richardson S, et al. Expert Clinician Certainty in Diagnosing Autism Spectrum Disorder in 16-30-Month-Olds: A Multi-site Trial Secondary Analysis. J Autism Dev Disord 2022: 1-16.
59. Reisinger DL, Hines E, Raches C, Tang Q, James C, Keehn RM. Provider and Caregiver Satisfaction with Telehealth Evaluation of Autism Spectrum Disorder in Young Children During the COVID-19 Pandemic. J Autism Dev Disord 2022; 52(12): 5099-113.
60. Charalampopoulou M, Choi EJ, Korczak DJ, et al. Mental health profiles of autistic children and youth during the COVID-19 pandemic. Paediatr Child Health 2022; 27(Suppl 1): S59-S65.
61. Evers K, Gijbels E, Maljaars J, et al. Mental health of autistic adults during the COVID-19 pandemic: The impact of perceived stress, intolerance of uncertainty, and coping style. Autism 2022: 13623613221119749.
62. Baribeau DA, Vigod SN, Pullenayegum E, et al. Developmental cascades between insistence on sameness behaviour and anxiety symptoms in autism spectrum disorder. Eur Child Adolesc Psychiatry 2022.
63. Stewart Campbell A, Needham BD, Meyer CR, et al. Safety and target engagement of an oral small-molecule sequestrant in adolescents with autism spectrum disorder: an open-label phase 1b/2a trial. Nature Medicine 2022; 28(3): 528-34.
64. Mournet AM, Wilkinson E, Bal VH, Kleiman EM. A systematic review of predictors of suicidal thoughts and behaviors among autistic adults: Making the case for the role of social connection as a protective factor. Clin Psychol Rev 2022; 99: 102235.
65. Lampinen LA, Zheng S, Taylor JL, et al. Patterns of sleep disturbances and associations with depressive symptoms in autistic young adults. Autism Res 2022; 15(11): 2126-37.
66. Safar K, Vandewouw MM, Pang EW, et al. Shared and Distinct Patterns of Functional Connectivity to Emotional Faces in Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder Children. Front Psychol 2022; 13: 826527.
67. Schachar RJ, Dupuis A, Arnold PD, et al. Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder: Shared or Unique Neurocognitive Profiles? Res Child Adolesc Psychopathol 2022.
68. Carter Leno V, Wright N, Pickles A, et al. Exposure to family stressful life events in autistic children: Longitudinal associations with mental health and the moderating role of cognitive flexibility. Autism 2022; 26(7): 1656-67.
69. Lei J, Charman T, Leigh E, Russell A, Mohamed Z, Hollocks MJ. Examining the relationship between cognitive inflexibility and internalizing and externalizing symptoms in autistic children and adolescents: A systematic review and meta-analysis. Autism Res 2022; 15(12): 2265-95.
70. Forbes G, Kent R, Charman T, Baird G, Pickles A, Simonoff E. How do autistic people fare in adult life and can we predict it from childhood? Autism Research 2022; n/a(n/a).
71. Pham HH, Sandberg N, Trinkl J, Thayer J. Racial and Ethnic Differences in Rates and Age of Diagnosis of Autism Spectrum Disorder. JAMA Netw Open 2022; 5(10): e2239604.
72. Kalb LG, Singh V, Hong JS, et al. Analysis of Race and Sex Bias in the Autism Diagnostic Observation Schedule (ADOS-2). JAMA Netw Open 2022; 5(4): e229498.
73. DuBay M. Cultural Adaptations to Parent-Mediated Autism Spectrum Disorder Interventions for Latin American Families: A Scoping Review. Am J Speech Lang Pathol 2022; 31(3): 1517-34.
74. Vanegas SB, Duenas AD, Kunze M, Xu Y. Adapting parent-focused interventions for diverse caregivers of children with intellectual and developmental disabilities: Lessons learned during global crises. J Policy Pract Intellect Disabil 2022; na: 1-13.
75. Steinbrenner JR, McIntyre N, Rentschler LF, et al. Patterns in reporting and participant inclusion related to race and ethnicity in autism intervention literature: Data from a large-scale systematic review of evidence-based practices. Autism 2022; 26(8): 2026-40.
76. Williams EG, Smith MJ, Boyd B. Perspective: The role of diversity advisory boards in autism research. Autism 2022: 13623613221133633.
77. Reetzke R, Singh V, Hong JS, et al. Profiles and correlates of language and social communication differences among young autistic children. Front Psychol 2022; 13: 936392.
78. Buijsman R, Begeer S, Scheeren AM. ‘Autistic person’ or ‘person with autism’? Person-first language preference in Dutch adults with autism and parents. Autism 2022: 13623613221117914.
79. Monk R, Whitehouse AJO, Waddington H. The use of language in autism research. Trends Neurosci 2022; 45(11): 791-3.
80. Bury SM, Jellett R, Haschek A, Wenzel M, Hedley D, Spoor JR. Understanding language preference: Autism knowledge, experience of stigma and autism identity. Autism 2022: 13623613221142383.
81. Keating CT, Hickman L, Leung J, et al. Autism-related language preferences of English-speaking individuals across the globe: A mixed methods investigation. Autism Res 2022.
82. Singer A, Lutz A, Escher J, Halladay A. A full semantic toolbox is essential for autism research and practice to thrive. Autism Res 2022.

